Meningeal Syndrome

Meningeal syndrome is not a disease in itself, but a combination of symptoms that indicate the existence of some pathological process in the meninges. The causes can be varied, but as a rule we must say that they always require immediate action.
In medicine, a syndrome is something that defines a group of signs and symptoms that occur together and are capable of responding to various etiologies. This means that a syndrome can be caused by a variety of illnesses.
In meningeal syndrome, the baseline set of symptoms consists of three phenomena:
- headache: headache
- Muscle rigidity: due to muscle contractures
- Fever: which may or may not be present, depending on whether it is infectious or not
Symptoms are evident in a patient when the meninges are already inflamed. The meninges are three very thin layers that cover the structures of the central nervous system within the skull and spine. As if they were a paper, meninges involve the brain and spinal cord.
There are three meninges: dura mater, pia mater, and arachnoid. Meningeal syndrome responds to inflammation of the last two, which anatomy describes as leptomeninges. When these layers become inflamed, they irritate the central nervous system.
Causes of meningeal syndrome
Although there are several causes capable of triggering this syndrome, the most important ones are divided into two groups: inflammatory and non-inflammatory. This general division does not determine the severity of the clinical picture, as we will see below.
Inflammatory causes
Among the inflammatory causes, we can mention:
- Bacteria: Perhaps the most important and known is meningococcal, a microorganism for which there is specific vaccination capable of preventing the meningitis it causes. Once the bacteria are installed, meningeal syndrome is usually complete, with all symptoms. It is also capable of causing outbreaks or epidemics in populations that maintain contact, which is why precautionary measures are extreme when a case is detected and confirmed.
- Viruses: Viral meningoencephalitis has a more insidious clinical presentation and ranges from relatively common viruses to rare microorganisms that cause specific diseases with first and last names.
- Fungi: A mycotic meningeal syndrome is rare but very aggressive. It usually occurs in people who have an immune deficiency who, because of their weakened defenses, become more prone to fungal attack. Treatment is also more complicated.
- Parasites: Parasitic meningitis is even more uncommon and there are only three microorganisms that lurk behind almost all cases. Transmission occurs from animals to humans, so the risk is greater for rural workers.

Non-Inflammatory Causes
The other causes are non-inflammatory, including:
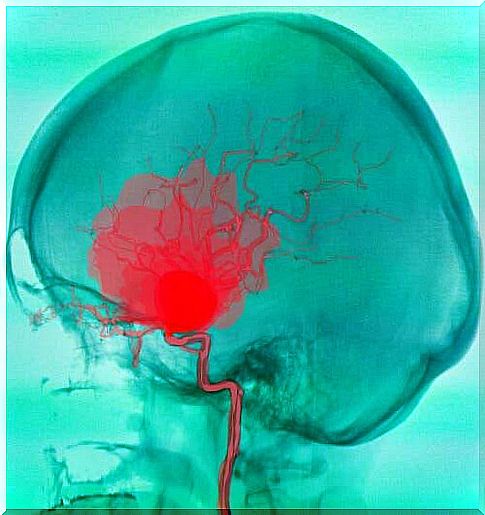
- Bleeding: When a stroke occurs due to a ruptured artery in the brain, the bleeding forms a collection of blood that, if located near the meninges, inflames them. The result is meningeal syndrome. Early in symptoms, a stroke can be confused with bacterial meningitis, including the presence of fever.
- Trauma: A head trauma, from shock or accident, can inflame the meninges. Several traumatic mechanisms can cause the accumulation of inflammatory fluid between the brain and the leptomeninges, irritating them.
- Neoplasms: Many tumors of the brain, cerebellum, and bone marrow do not start with more obvious signs than meningeal syndrome. The malignant mass pushes the meninges and ends up irritating them, sometimes without putting pressure on other structures.
How to recognize meningeal syndrome?
As fever is not always present in meningeal syndrome, there are two symptoms that are considered to constitute it: headache and muscle contractures.
The headache in these cases is a pain that tends to be intense and persistent. It is not uncommon for the patient to scream because of the pain in the skull. The predominant sites are the frontal and occipital regions, that is, at the level of the forehead or near the nape of the neck.
This headache is usually accompanied by an intensification when faced with stimuli such as light or noise. When intensified by light, it is called photophobia, and the person is forced to close their eyes. When the pain is worse in the presence of sounds, it is called algiacusis.
The other feature is muscle contractures. In the syndrome in question, the muscles of the neck, back and lower limbs can become tight and rigid. The rigidity of the back of the neck does not allow the chin to be brought to the chest, for example, while the back does not allow the knees to be brought to the chest. These are historical and classic signs that medicine has associated with meningitis for decades.
Faced with these symptoms, it is essential to consult a doctor without delay. The provider will order the necessary blood tests and nervous system imaging, including a lumbar puncture to study the cerebrospinal fluid, if necessary. Obviously, this is not a picture that can be overlooked, given the risk involved.